Abstract
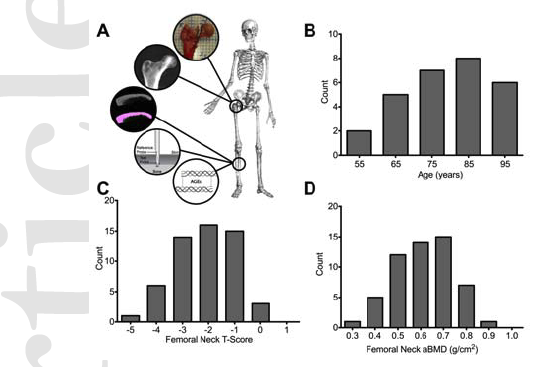
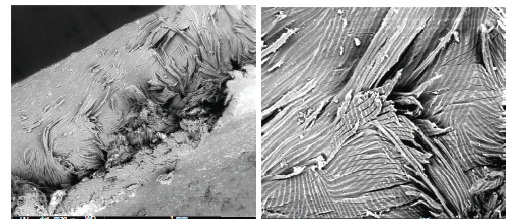
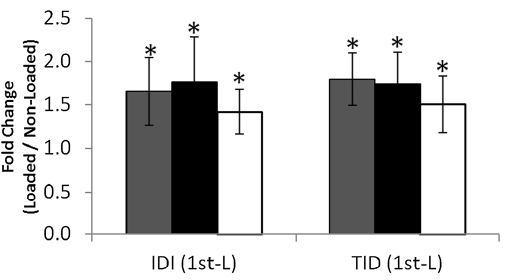
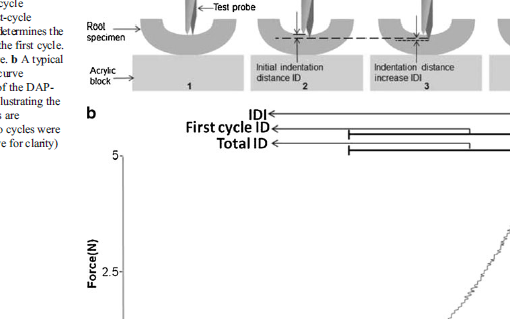
The diagnosis of fracture risk relies almost solely on quantifying bone mass, yet bone strength is governed by factors at multiple scales including composition and structure that contribute to fracture resistance. Furthermore, aging and conditions such as diabetes mellitus alter fracture incidence independently of bone mass. Therefore, it is critical to incorporate other factors that contribute to bone strength in order to improve diagnostic specificity of fracture risk. We examined the correlation between femoral neck fracture strength in aging female cadavers and areal bone mineral density, along with other clinically accessible measures of bone quality including whole-bone cortical porosity (Ct.Po), bone material mechanical behavior measured by reference point indentation (RPI), and accumulation of advanced glycation end-products (AGEs). All measurements were found to be significant predictors of femoral neck fracture strength, with areal bone mineral density (aBMD) being the single strongest correlate (aBMD: r = 0.755, p < 0.001; Ct.Po: r = -0.500, p < 0.001; RPI: r = -0.478, p < 0.001; AGEs: r = -0.336, p = 0.016). RPI-derived measurements were not correlated with tissue mineral density or local cortical porosity as confirmed by micro-computed tomography (μCT). Multiple reverse stepwise regression revealed that the inclusion of aBMD and any other factor significantly improve the prediction of bone strength over univariate predictions. Combining bone assays at multiple scales such as aBMD with tibial Ct.Po (r = 0.835; p < 0.001), tibial difference in indentation depth between the first and 20th cycle (IDI) (r = 0.883; p < 0.001), or tibial AGEs (r = 0.822; p < 0.001) significantly improves the prediction of femoral neck strength over any factor alone, suggesting that this personalized approach could greatly enhance bone strength and fracture risk assessment with the potential to guide clinical management strategies for at-risk populations.
https://www.ncbi.nlm.nih.gov/pubmed/26060094
J Bone Miner Res. 2015 Dec;30(12):2207-14. doi: 10.1002/jbmr.2568. Epub 2015 Jul 14.